Sitting for Long Hours Affects Blood Circulation and Leg Health in Working People
Dr JK Avhad MBBS MD [Last updated 24.12.2025]
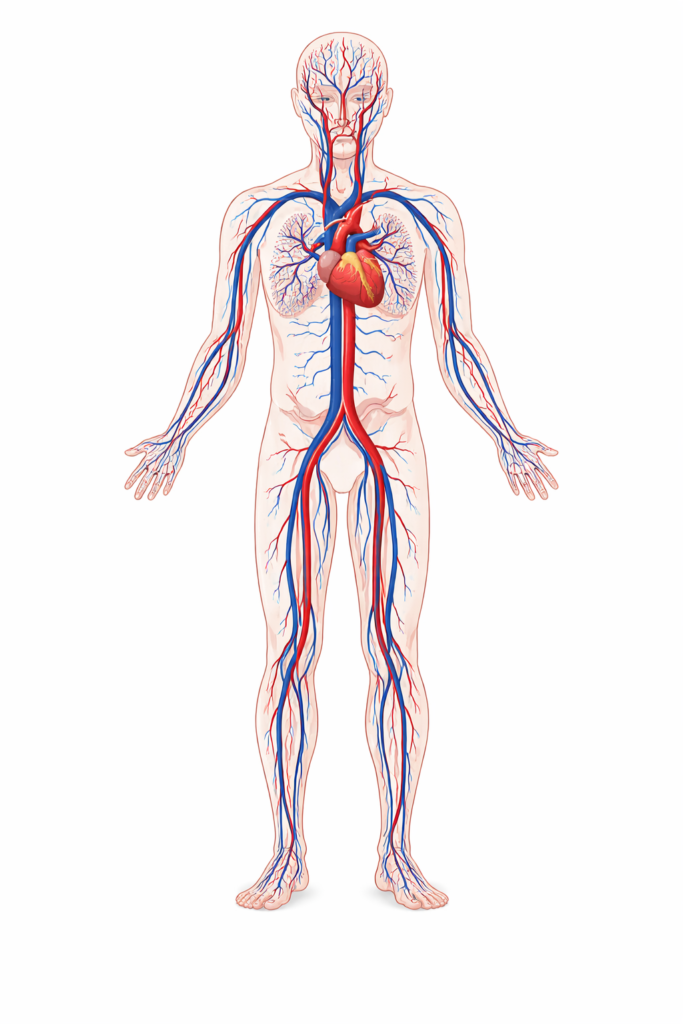
Long hours of sitting—at desks, in trucks, at call centers, in clinics, and on long commutes—can quietly harm blood circulation and leg health in working Americans. When you sit still for prolonged periods, calf-muscle pumping slows, venous return decreases, and blood pools in the lower legs. Over the time, this can contribute to ankle swelling, heaviness, varicose veins, skin changes, and in higher-risk situations, blood clots such as deep vein thrombosis (DVT).
If you work in the United States today, chances are you sit—often for hours at a time. Office jobs, telework, driving-based work, and long screen-heavy shifts can turn the body into a “still machine.” The issue is not that sitting is evil; it’s that uninterrupted sitting is unnatural for circulation.
National data show that a large share of U.S. adults spend many hours seated daily, and the CDC estimates that up to 900,000 Americans are affected by venous thromboembolism (VTE) each year.
Circulation responds quickly to small, consistent movement, you don’t need a gym routine to protect your legs—you need frequent circulation breaks.
When you sit motionless, several mechanical and physiological changes happen:
- Hip and knee flexion compresses veins and slows venous flow.
- The calf muscle pump (your “second heart”) is largely inactive.
- Gravity promotes blood pooling in lower legs and feet.
- Microcirculation can slow, contributing to swelling and tissue pressure.
Why sitting slows the “calf pump”
The calf muscles squeeze deep veins when you walk or flex your ankle. This action pushes blood upward against gravity toward the heart.
When you sit still:
- Calves don’t contract enough,
- Blood moves more slowly,
- Veins carry more volume under higher pressure.
Veins contain one-way valves. Persistent pooling increases pressure and can gradually worsen valve function, contributing to:
- Varicose veins,
- Chronic venous insufficiency,
- Skin discoloration around ankles
Varicose veins and chronic venous insufficiency are not caused by sitting alone—genetics, pregnancy history, age, and body weight matter too. But long, uninterrupted sitting can worsen venous pressure and symptoms:
- Heaviness,
- Aching after work,
- Swelling that improves overnight,
- Restless legs sensations.
Venous stasis is not always dramatic. It can look like:
- Tight shoes by evening,
- Socks imprints,
- Mild ankle puffiness,
- A dull ache behind the knees.
A major concern with long immobility is venous thromboembolism (VTE), which includes:
- Deep vein thrombosis (DVT): Clot in the deep veins, usually legs
- Pulmonary embolism (PE) : Clot travels to the lungs
The CDC estimates up to 900,000 people in the U.S. are affected by VTE each year, and 60,000–100,000 Americans die annually from VTE. (CDC)
Sitting increases clot risk
Clot risk rises when the body meets the classic “Virchow’s triad” conditions:
- Stasis (slow blood flow)
- Endothelial irritation
- Hypercoagulability (blood more prone to clot)
Prolonged sitting mainly drives stasis, especially if combined with dehydration, recent illness, or high-risk medical conditions.
Research has linked prolonged seated immobility—at work or with extended sitting—to increased DVT/VTE risk in certain contexts.
This article focuses on legs, but circulation is whole-body.
- Long sedentary time is associated with higher cardiometabolic risk overall in adult. (NCBI)
- Inactivity prevalence remains substantial in the U.S. adult population. (CDC)
Office and remote workers
- Back-to-back calls
- Few natural walking breaks
- Lunch at the keyboard
Drivers, delivery, and trucking
- Long seated hours
- Vibration, limited leg movement
- Fewer bathroom breaks leads to dehydration risk
Healthcare and lab roles
Surprisingly, healthcare workers can also be highly sedentary due to charting and computer tasks.
Common symptoms
- Ankle swelling that improves overnight
- Heaviness or aching calves after long shifts
- Pins and needles sensation from nerve compression
- Restless legs at night
- Visible veins becoming more prominent
Red flags
- Sudden one-leg swelling (especially calf)
- Calf pain/tenderness, warmth, redness
- New shortness of breath, chest pain, coughing blood
Protect circulation at work
Instead of one long workout, use micro-movements:
Every 30–60 minutes (1–2 minutes):
- 10–20 calf raises
- 10 ankle circles each direction
- 10 seated knee extensions (straighten leg, flex foot)
- Stand up, take 20–40 steps
Desk setup tips
- Avoid crossing legs for long periods
- Keep feet flat or use a small footrest
- Consider a timer or watch reminder
If you use a standing desk
Standing can reduce sitting time, but static standing isn’t the solution. Alternate positions and add movement.
What to do for leg swelling after work
Same-day relief
- 10–15 minutes with legs elevated above heart level
- gentle ankle pumping while elevated
- light walk after dinner
- hydration (especially if you had lots of caffeine)
Compression stockings
Graduated compression can help symptoms for many people with swelling or varicose veins. If you have diabetes, arterial disease, or neuropathy, discuss with a clinician first.
How to reduce clot risk during long sitting
- Move: stand and walk briefly every hour
- Hydrate: dehydration increases blood viscosity
- Avoid constrictive clothing around thighs/waist for long sitting
- Know your risk: recent surgery, cancer treatment, pregnancy/postpartum, prior clots—these raise risk substantially. (CDC)
WHO guidelines recommend that adults limit sedentary time and replace it with physical activity of any intensity, with additional benefits from more moderate-to-vigorous activity.
FAQs
Q. Do long hours of sitting cause varicose veins?
They can worsen symptoms and venous pressure, especially if you are genetically prone. Varicose veins are multifactorial, but movement breaks help.
Q. How often should I stand up for circulation?
A practical target is every 30–60 minutes, even for 1–2 minutes.
Q. Are leg cramps at night related to sitting all day?
Sometimes. Reduced daytime calf activation, dehydration, and electrolyte factors can contribute. Gentle evening walking and calf stretching can help.
Q. Does walking after meals help circulation?
Yes. A 10–15 minute walk supports calf pumping and overall metabolic health.
Q. When should I worry about a blood clot?
If swelling is one-sided, painful, warm/red, or if you have chest symptoms (shortness of breath, chest pain), seek urgent evaluation.
Conclusion
Sitting is part of modern American work—but unbroken sitting is not. Prolonged seated hours reduce venous return, promote leg pooling, increase swelling and heaviness, and—when combined with other risk factors—can raise the likelihood of serious clotting events. That is why the most effective strategy is also the simplest: break up sitting frequently. Your legs don’t need a dramatic overhaul; they need regular pumping.
This article is for informational purpose only and does not substitute for professional medical advise. For proper diagnosis and treatment seek the help of your healthcare provider.
References:
- Centers for Disease Control and Prevention. (2025). Data and Statistics on Venous Thromboembolism (Blood Clots). CDC
- Centers for Disease Control and Prevention. (2025). Adult Physical Inactivity Outside of Work. CDC
- World Health Organization. (2020). WHO guidelines on physical activity and sedentary behaviour. World Health Organization
- World Health Organization. (2024). Physical activity (Fact sheet). World Health Organization
- Bull, F. C., et al. (2020). World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicine, 54(24), 1451–1462. bjsm.bmj.com
- National Center for Biotechnology Information. (2020). Recommendations—WHO Guidelines on Physical Activity and Sedentary Behaviour. NCBI
- Healy, B., et al. (2010). Prolonged work- and computer-related seated immobility and risk of venous thromboembolism. Journal of the Royal Society of Medicine. PubMed Central
- Johannesen, C. D. L., & colleagues. (2020). Sedentary work and risk of venous thromboembolism. Scandinavian Journal of Work, Environment & Health. SJWEH
- Matthews, C. E., et al. (2021). Sedentary Behavior in United States Adults: Fall 2019. American Journal of Preventive Medicine. PubMed Central
- Stella, S. Y., et al. (2015). Self-Reported Sitting Time in New York City Adults. Preventing Chronic Disease, 12, E165. CDC
- Beckman, M. G., et al. (2010). Venous thromboembolism: A public health concern. American Journal of Preventive Medicine. ScienceDirect
- Centers for Disease Control and Prevention. (2015). A review of estimated attributable healthcare costs (VTE). CDC Stacks
- Suadicani, P., et al. (2012). Jobs encompassing prolonged sitting in cramped positions and risk of DVT. Journal of Thrombosis and Haemostasis. PubMed Central
- Chen, L., et al. (2023). Leisure sedentary behaviour and risk of venous thromboembolism. Frontiers in Cardiovascular Medicine. PubMed Central
- JAMA. (2012). Venous thromboembolism in adult hospitalizations. JAMA. JAMA Network
- National Library of Medicine (NIH). (2018). Americans sit too much, CDC says (Behind the Headlines). NCBI
- Okely, A. D., et al. (2021). 2020 WHO guidelines on physical activity and sedentary behaviour. Journal of Sport and Health Science. ScienceDirect
- Pope, C. A., et al. (2015). Fine particulate air pollution and mortality. New England Journal of Medicine. PubMed Central
- U.S. Department of Health and Human Services. (2018). Physical Activity Guidelines for Americans (2nd ed.).
- National Heart, Lung, and Blood Institute. (n.d.). Healthy movement and cardiovascular health resources.
- American Heart Association. (n.d.). Sedentary behavior and heart health statements.
